The health of our gut is a strong indicator of our overall wellbeing as the functioning of our GI tract impacts metabolism, the immune system, and hormonal activity. The gastrointestinal and hormonal systems are closely intertwined and mutually dependent. Any disruption in their relationship may result in a health problem that requires a holistic approach.
This article explains the connection between the gut and hormones and provides practical advice on how to restore gut health and achieve hormonal balance.

The gut microbiome contains trillions of bacteria, fungi, and other microorganisms that reside in your intestinal tract, mainly in the large intestine (colon). This microbial diversity is crucial for physical, mental, and hormonal health.
Hormonal imbalance can indicate a disrupted microbiome or dysbiosis. Other signs of an unhealthy gut include digestive issues (e.g., bloating, constipation, diarrhea), food allergies and sensitivities, weight oscillations, autoimmune conditions, skin inflammation, and fatigue.
Beneficial gut bacteria perform several vital functions that influence multiple physiological processes, including hormone activity:
It is important to remember that the gut and hormones are inextricably linked and disruptions to one system affect the other. In a complex interplay, hormones support gut function and any hormonal disruption can upset the stomach, cause constipation, cramping, gas, bloating, acid reflux, and other more serious issues.
An imbalanced microbiota potentially contributes to hormonal imbalance via various mechanisms that are still being studied. It is believed that problems with the microbiome can contribute to the following medical conditions:
Hormonal changes directly interfere with the digestive processes in the body and impact gut health. Hormones can cause digestive organs to empty at a faster or slower rate than usual.
Women are more prone to gastrointestinal problems because female-specific hormones (progesterone and estrogen) are more likely to cause gut issues. These changes can occur in healthy women during puberty, menstruation, PMS, pregnancy, or menopause as the result of too much estrogen or progesterone in the system.
Disrupted hormonal activity may provoke the following gut issues:
The following hormones are especially closely tied to the gut:
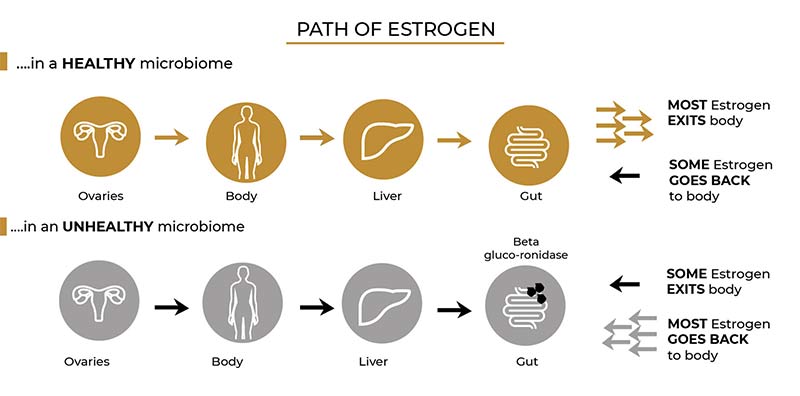
The gut plays a crucial role in estrogen metabolism. GI microbes regulate circulating estrogen levels and modulate estrogen-dependent physiological processes. Moreover, the gut contains many estrogen receptors that influence gut motility and sensitivity.
An imbalanced gut microbiome can disrupt estrogen metabolism and lead to estrogen dominance, resulting in painful periods, PMS, endometriosis, or polycystic ovary syndrome (PCOS).
Some menopausal and perimenopausal women experience digestive problems that scientists think might be caused by dramatic hormonal shifts. These include heartburn, bloating, constipation, and irritable bowel syndrome (IBS).
Progesterone can inhibit gut motility, especially during the menstrual cycle, leading to slower bowel movements and constipation. This hormone increases the risk of acid reflux, a common issue experienced during pregnancy due to elevated progesterone levels.
High cortisol levels can limit gut motility, cause inflammation of the digestive tract, and increase sensitivity, leading to diarrhea or irritable bowel syndrome (IBS). Furthermore, excess cortisol due to chronic stress can suppress the immune system, shutting down the body’s anti-inflammatory response and compromising gut health in the long run.
Note: Learn how to lower cortisol levels naturally to maintain a healthy gut flora.
You can experience hypothyroidism (underactive thyroid) due to gut issues, even if your thyroid gland is working optimally because nearly 20% of thyroid hormone conversion occurs in the gut.
Conversely, a malfunctioning thyroid gland negatively affects metabolism, disrupting nutrient absorption and leading to constipation (hypothyroidism) or diarrhea (hyperthyroidism). An impaired thyroid can also cause inflammation and a “leaky gut”.
Note: Learn how to reduce inflammation and alleviate its numerous side effects.
Testosterone and digestion are inextricably linked. Low testosterone levels can cause gastritis, leaky gut, irritable bowel syndrome.
Testosterone is essential for gut function in the following ways:
Insulin resistance and type 2 diabetes are conditions that are characterized by chronically high blood sugar levels. Continually elevated blood sugar levels negatively impact the microbiota, causing dysbiosis, impacting nutrient absorption, and leading to multiple gastrointestinal conditions (such as intestinal bloating, nausea, vomiting, diarrhea, flatulence, constipation, etc.).
Note: Learn how weight loss can help reverse insulin resistance.
Ghrelin is a hormone mainly synthesized in the stomach that plays a vital role in signaling hunger to the brain. The gut microbiota may influence ghrelin levels, thereby impacting appetite and energy metabolism.
Ghrelin affects gut health by maintaining the integrity of the gut barrier and regulating intestinal motility and gastric emptying. Research also shows that ghrelin levels are negatively affected by stress.
Abnormal levels of ghrelin are associated with intestinal disorders such as IBS, gastroesophageal reflux (GERD), and gastroparesis.
This stomach-produced peptide hormone plays a pivotal role in digestive health. Its key responsibilities are the following:
Gastric acid juice prevents infectious agents from reaching the intestine and helps break down the food we eat.
Excess cortisol triggered by stress may dysregulate gastrin function and contribute to stomach acid imbalance or acid reflux. Imbalanced gastrin production may lead to stomach pain, diarrhea, heartburn, bleeding, weight loss, or infections.
Cholecystokinin (CCK) is a peptide hormone responsible for digestion, appetite control, and nutrient absorption.
This hormone is released in the small intestine and the brain. Thus, its impact on the central nervous system, gut health, and other hormones is twofold. Some studies suggest that CCK may also influence cognitive function and modulate stress-related behavior (e.g., panic attacks, anxiety, etc.).
CCK performs the following digestive functions:
This GI hormone regulates digestive processes by maintaining pH balance in the small intestine and pancreas, inhibiting the production of gastric acid, and preventing too much acidity.
Secretin’s vital physiological functions are the following:
The bidirectional relationship between the gut and hormones requires a multifaceted approach. You can start small and tweak your daily habits to improve your hormonal status and gut health or seek professional medical help for more advanced medical solutions.
“You are what you eat” is a scientifically backed statement that explains many hormonal irregularities and gut issues resulting from poor food choices.
In general, a diverse diet rich in fresh and free from processed foods promotes the growth of beneficial gut bacteria and improves overall health.
Follow these guidelines to nurture a healthy, diverse gut microbiome and gain hormonal stability:
Note: Omega-3 fatty acids benefit more than just the gut. Discover the benefits of omega-3 for the skin.
Chia seeds are one of the most popular omega-3-rich foods, which is why they are praised by skin experts. Learn more about the benefits of chia seeds for the skin.
As an addition to a balanced diet, doctors recommend hormone-balancing vitamins and supplements that can help to correct nutritional deficiencies and alleviate hormone-triggered sweating, insomnia, reduced sex drive in men and women, hair loss, or acne.
You can improve gut function and restore hormonal balance with a hormone detox, vitamin B12 injections, IV therapy, or some of the following gut-supporting supplements*:
Note: Discover the 10 best vitamins for an immune system boost. Learn more about the benefits of vitamin C, vitamin D, and vitamin B IV treatments.
| *Disclaimer These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease. |
Small adjustments in your daily life can improve overall health, boost digestion, and stabilize the hormones. The most beneficial lifestyle changes for gut and hormone health include the following:
Keeping your weight in check is vital in preventing hormone-triggered disorders, such as obesity, diabetes, or thyroid dysfunction. These conditions disrupt appetite regulation and metabolic health, leading to low-grade inflammation and impaired digestive function.
Medical weight loss programs are an effective way to reduce hormonal belly fat and tackle hormonal weight gain or weight loss. These treatment plans are tailored for each patient and provide long-term, sustainable results. Doctors advise against fad diets that can be ineffective and compromise your gut microbiota.
Some household and cosmetic products contain a toxic chemical called xenoestrogen – a synthetically produced estrogen typically found in plastics, pesticides, and fragrances. This substance can disrupt the endocrine system and interfere with hormone receptors.
Reduce the use of plastic and choose organic, eco-friendly products to minimize the negative impact of the “foreign” estrogen from the environment. Also try to consume hormone-free meat products and purchase food items in glass or steel containers to reduce the risk of ingesting xenoestrogen.
Bioidentical hormone replacement therapy (BHRT) corrects hormonal deficiencies using artificial hormones that are structurally identical to estrogen, progesterone, and testosterone.
BHRT can alleviate hormone-triggered conditions, including insomnia, sweating, low libido, brain fog, anxiety, and depression.
Lower microbial diversity is in direct correlation with lower estrogen levels in women. Recent studies confirm BHRT’s beneficial impact on the gut microbiome during menopause and in patients diagnosed with premature ovarian insufficiency (POI).
Furthermore, BHRT patients report fewer gut-related issues, such as bloating, constipation, or diarrhea. The treatment regulates shifting gastrointestinal hormones, decreasing the risk of irritable bowel syndrome (IBS).
Testosterone therapy restores optimal testosterone levels in men and women and provides numerous benefits, including more energy, increased sex drive, and weight loss.
There is a strong connection between testosterone and gut health, too. TRT can alleviate many digestive problems by optimizing testosterone activity.
A healthcare provider might prescribe medication to provide temporary relief from an upset stomach or treat the underlying hormonal problem. The choice depends on the patient’s symptoms, medical record, and overall health.
Over-the-counter (OTC) medicine for digestive issues include antacids such as Tums or Rolaids (heartburn, sour stomach), Pepto-Bismol (diarrhea, nausea), and Mylanta (heartburn, sour stomach, bloating).
Treatment options for hormone imbalances include hormone replacement medication, birth control methods (e.g., pill, ring, patch, IUD, etc.), metformin, thyroid medication, and others.
Note: Besides hormone balancing, metformin is a medication commonly used for weight loss. Find out if metformin aids weight loss.
You can restore a healthy balance of gut bacteria by regulating hormones through lifestyle changes, supplementation, diet, or hormone replacement therapies. A well-balanced gut microflora is indispensable for physical, mental, and emotional wellbeing. Prioritizing digestive health is essential for optimal hormonal activity and strong immunity.
Consult the Vibrant Vitality Clinic experts for more information on maintaining gut function and rebalancing hormones.



4325 E Indian School Rd, Suite 130
Phoenix, AZ 85018
United States
(480) 422-2058
info@vibrantvitalityclinic.com
Monday - Friday: 9:00 am - 6:00 pm
Saturday: 9:00 am - 3:00 pm
Sunday: Closed
